Abstract
Intracranial bleeding, either at presentation or during induction, is associated with early deaths in acute promyelocytic leukemia (APL). With ATRA and chemotherapy treatment, prior CNS hemorrhage is a risk factor for a subsequent CNS relapse (18.7% risk at 5 years, Montesinos P, et al. Haematologica 2009). However, it is not known if this remains true with the advent of upfront arsenic trioxide (ATO) based regimens. At our center, we have used an upfront ATO-based APL treatment regimen for over two decades. From 1998 to 2015, single agent ATO was used (Mathews V et al. JCO 2010), while after 2015, a combination of ATRA and ATO with minimal anthracyclines (Kulkarni U et al. BCJ 2022), was used. We conducted a retrospective analysis of all patients with newly diagnosed APL, who either presented with intracranial bleeding or developed intracranial bleeding during induction, from January 1998 to May 2022.
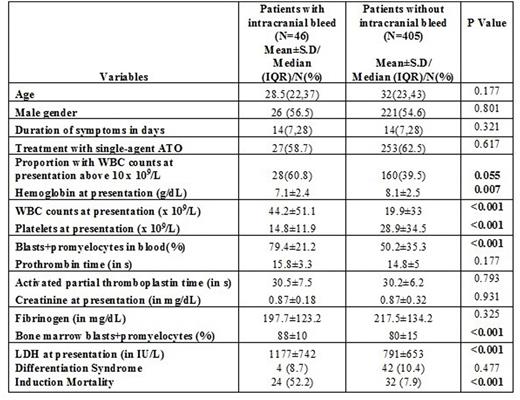
A total of 488 patients (288 treated with single agent ATO and 200 with ATO, ATRA, and minimal anthracyclines) were treated during the study period. Of these, we excluded the 37 cases (3 were treated at relapse, 8 had received partial treatment elsewhere, 21 were discharged against medical advice without evidence of intracranial bleeding during induction, and 5 are currently on induction therapy at the time of this analysis). Of the remaining 451 patients treated for newly diagnosed APL at our center, 32 (7.1%) patients had presented with an intracranial bleed, while another 14 (3.1%) patients developed intracranial bleeding during induction therapy. Their characteristics (n=46) are shown and compared with the rest of the cohort without intracranial bleed (n=405) in the table below. Patients with intracranial bleed had lower hemoglobin, higher WBC counts, lower platelet counts, higher LDH, higher blasts + promyelocytes in blood and marrow and higher induction mortality than those without intracranial bleed.
Of the 32 patients who presented intracranial bleeding, 13 (40.6%) died during induction, one patient was discharged against medical advice, and the remaining 18 survived and were in morphologic remission at the end of induction.
Of the 14 patients who developed intracranial bleeding during induction therapy at a median of day 4 (IQR: 4 to 15 days), 10 (71.4%) died during induction therapy, one was discharged against medical advice, while the remaining three survived and were in morphologic remission at the end of induction.
Thus, a total of 21 of 46 patients (45.7%) had intracranial bleeding either at presentation or during induction and were in morphologic remission at the end of induction. At a median follow-up of 56 months (IQR: 22.3 to 78.0), there were 2 (9.5%) relapses and one death while in remission in this cohort. This group (n=21) had a comparable event-free survival (event defined as death or relapse) as compared to patients who did not have intracranial bleeding and were in remission following induction (n=372) (5-year EFS 77.8% ± 12.2% v/s 77.4% ± 2.4%, log-rank p 0.701).
Thus, with the use of upfront ATO-based regimens, intracranial bleeding in APL is associated with early mortality during induction therapy, while it does not seem to be associated with increased relapse risk in patients who survive induction therapy.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal